What Is The History Of Scleroderma? Tracing A Complex Condition Through Time
Understanding the journey of a medical condition can offer so much comfort and insight, particularly when you or someone you care about is living with it. Scleroderma, a condition that makes the skin and sometimes internal organs feel tight and hard, has a long and rather winding story of discovery. Knowing its past helps us appreciate just how far we have come in understanding this challenging illness.
For a very long time, medical professionals and healers simply did not know what to make of the unusual changes they saw in people's bodies. It was a mystery, really, with symptoms that were hard to pin down and connect. People experienced these physical changes, but the reasons behind them were completely hidden from view.
This article will take you through the fascinating history of scleroderma, from its earliest, hazy mentions to the sophisticated understanding we have today. We will look at how different people, over many centuries, slowly pieced together the puzzle of this condition, so you can see the progress for yourself.
Table of Contents
- Early Glimpses: The First Recorded Observations
- Naming the Condition: The 18th and 19th Centuries
- The 20th Century: Deeper Understanding and Classification
- Modern Era: Advances and Ongoing Challenges
- Frequently Asked Questions About Scleroderma's Past
- Conclusion
Early Glimpses: The First Recorded Observations
Ancient Accounts and Vague Mentions
The very earliest mentions of symptoms that sound a little like scleroderma are, in a way, quite hard to pin down. We find some descriptions in ancient medical writings that talk about skin hardening or thickening. These accounts, however, are very general and do not give us enough detail to say for sure that they were describing scleroderma as we know it today. It's almost like looking through a fog, trying to make out shapes.
For example, some historians point to writings from Hippocrates or even earlier, where conditions involving skin changes were noted. Yet, the language used was not precise, and there were no specific names for these unusual skin problems. So, it is that these early observations were more about general skin issues than any specific disease.
The lack of clear medical terms and detailed patient records from these times makes it a bit of a challenge to trace the exact beginnings. People simply did not have the tools or the knowledge to classify diseases in the way we do now. Therefore, any mention is more of a potential hint than a definite identification.
The Renaissance Era: A More Defined Picture Begins
The Renaissance, a time of great learning and discovery, started to bring a bit more clarity to medical observations. It was during this period that physicians began to record patient symptoms with greater care and detail. This improved approach allowed for more specific descriptions of various conditions, and scleroderma was apparently one of them.
One of the earliest descriptions that many medical historians agree upon comes from a doctor named Carlo Curzio. In 1753, he wrote about a young woman who had skin that was very hard and tight, making it difficult for her to move her body. This account is often seen as the first truly clear description of what we now call scleroderma. It gave others something more concrete to think about.
This particular case report was a significant step because it moved beyond general observations. It provided a detailed picture of a patient's experience, allowing future doctors to recognize similar patterns. It showed, too, that some medical minds were really starting to pay close attention to these unusual skin conditions.
Naming the Condition: The 18th and 19th Centuries
Alibert and the Term "Sclerodermie"
The 19th century was a very important time for naming and classifying diseases. It was then that Jean-Louis Alibert, a French dermatologist, actually gave the condition a name that stuck. In 1817, he used the term "sclerodermie" to describe the skin hardening he observed in patients. This name comes from two Greek words: "skleros," meaning hard, and "derma," meaning skin. It was a straightforward way to describe the main symptom.
Alibert's work helped to solidify the condition's identity within the medical community. Giving it a specific name made it easier for doctors to talk about it, to record cases, and to share their findings. This naming was a big step toward recognizing scleroderma as a distinct illness, something you know is important for any medical condition.
Before this, various terms might have been used, or the condition might have been lumped in with other skin problems. Alibert's contribution provided a common language, which is pretty essential for medical progress. It meant that doctors in different places could refer to the same condition with clarity.
Distinguishing Features and Clinical Recognition
As the 19th century continued, doctors began to notice that scleroderma was not just a skin problem. They started to see that it could affect internal organs too. This was a crucial realization, as it showed the condition was much more complex than initially thought. It meant it was a systemic disease, impacting the whole body, basically.
For example, in 1842, Dr. Thomas Addison, a British physician, described a patient with widespread skin hardening along with internal organ involvement. This observation helped medical professionals understand that the condition could be far more serious than just changes to the skin. It expanded the understanding of what scleroderma truly was.
These detailed clinical descriptions helped to separate scleroderma from other conditions that might have similar skin symptoms, like certain types of swelling or other connective tissue diseases. It was about refining the picture, making it clearer for doctors to diagnose. This period was all about getting a better handle on the condition's full scope.
The 20th Century: Deeper Understanding and Classification
Autoimmunity and Systemic Involvement
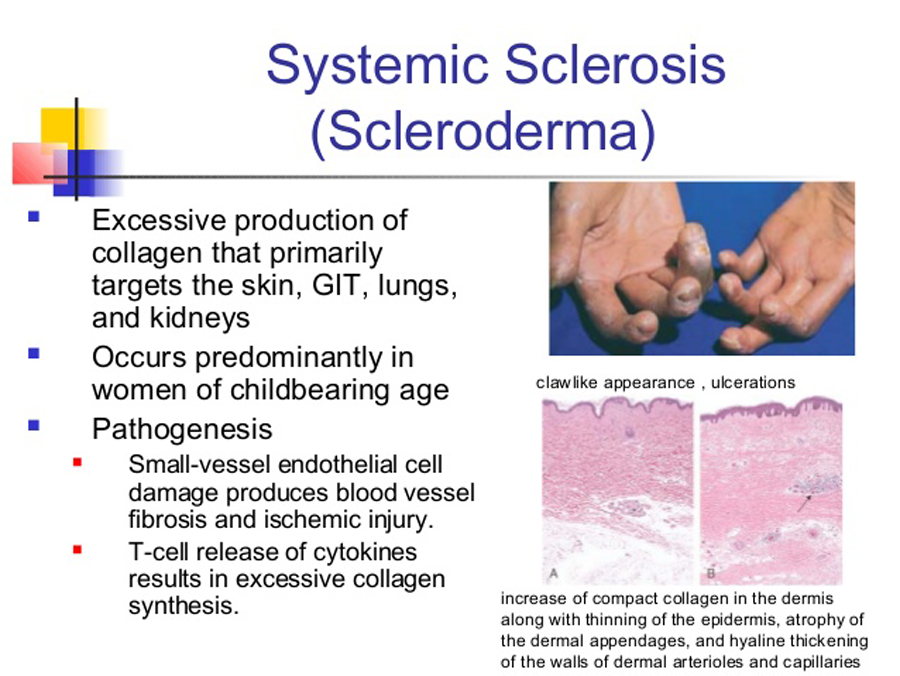
The 20th century brought a huge shift in medical understanding, especially concerning the immune system. Scientists began to realize that scleroderma was an autoimmune disease. This means the body's own immune system, which is supposed to protect us, sort of mistakenly attacks healthy tissues. This was a really big breakthrough.
This understanding helped explain why scleroderma could affect so many different parts of the body, not just the skin. It made sense that if the immune system was involved, it could cause problems in the lungs, heart, kidneys, and digestive system. This realization changed how doctors approached the condition, moving beyond just treating skin symptoms.
The concept of autoimmunity provided a framework for research, guiding scientists to look for specific antibodies in the blood that are characteristic of scleroderma. It was a pivotal moment, truly, in understanding the underlying mechanisms of the disease. This knowledge opened up entirely new avenues for investigation and potential treatments.
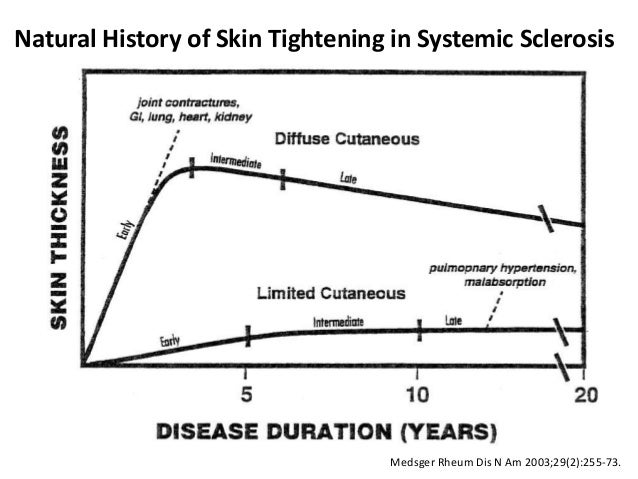
Subtypes and Diagnostic Progress
As the understanding of scleroderma grew, doctors began to recognize that it wasn't just one single condition. They saw that it presented in different ways, with varying degrees of severity and organ involvement. This led to the classification of scleroderma into different subtypes, such as limited cutaneous scleroderma and diffuse cutaneous scleroderma. This was a very helpful step for diagnosis and treatment planning.
The development of new diagnostic tools also played a big part. Blood tests became more sophisticated, allowing doctors to identify specific autoantibodies that are linked to scleroderma. For instance, the discovery of anti-centromere antibodies and anti-Scl-70 antibodies helped to distinguish between the different forms of the disease. I mean, this made a huge difference in how accurately doctors could identify the condition.
These classifications and improved diagnostic methods meant that patients could receive a more precise diagnosis, which is absolutely vital for getting the right care. It allowed medical teams to tailor treatments more effectively to the specific type of scleroderma a person had. This level of detail was a huge leap forward.
The Role of Research and Patient Advocacy
The 20th century also saw a significant increase in dedicated medical research into scleroderma. Scientists and doctors worked hard to understand the disease's causes, how it progresses, and what might help manage its effects. This ongoing research effort is really what drives progress in finding better treatments.
Alongside the scientific advancements, patient advocacy groups began to form. These groups played a crucial role in raising awareness about scleroderma, supporting research, and providing resources for patients and their families. They helped to give a voice to those living with the condition, which is so important for pushing for more research and better care.
These groups, like the Scleroderma Foundation, have been instrumental in funding studies and connecting people who have the disease. Their efforts have helped to make sure that scleroderma remains a focus for medical investigation. It shows how much good can come from people coming together for a common cause, right?
Modern Era: Advances and Ongoing Challenges
Genetic Insights and Biomarkers
In our current time, research into scleroderma has become even more advanced. Scientists are now looking deeply into the genetic factors that might make someone more likely to get the disease. Understanding these genetic links could open doors to new ways of preventing or treating the condition. It is a complex area, but full of promise.
The discovery of new biomarkers, which are measurable indicators of a biological state, is also a big step. These biomarkers can help doctors diagnose scleroderma earlier, predict how it might progress, and even tell if a treatment is working. This kind of precise information allows for more personalized care, which is very helpful for patients.
This detailed genetic and biomarker research is continually refining our understanding of scleroderma. It is helping us see the disease not as one single entity, but as a spectrum of conditions with different underlying mechanisms. This depth of knowledge is absolutely essential for future breakthroughs.
Targeted Therapies and Improved Outcomes
The understanding gained over centuries has led to the development of more targeted therapies for scleroderma. While there is still no single cure, treatments are now much better at managing symptoms and slowing the disease's progression. These therapies aim to address specific aspects of the disease, like inflammation or organ damage. This has led to significantly improved outcomes for many people.
For instance, medications that suppress the immune system or reduce fibrosis (the hardening of tissue) have made a real difference in the lives of patients. People are living longer and with a better quality of life than in previous decades. This progress is a direct result of all the historical research and observation.
The focus today is on finding even more effective and safer treatments. Researchers are exploring new drug candidates and treatment strategies all the time. This ongoing effort gives a lot of hope to those living with scleroderma, showing that progress is always happening.
The Future of Scleroderma Research
The story of scleroderma is still being written. Today, researchers are working on a wide range of promising areas. This includes developing new ways to detect the disease even earlier, perhaps before significant symptoms appear. They are also looking at very specific molecular pathways to find even more targeted therapies.
There is also a growing emphasis on personalized medicine. This means tailoring treatments to an individual's specific genetic makeup and disease characteristics. The goal is to make treatments as effective as possible for each person, reducing side effects and improving overall results. It's a very exciting time for medical science.
The hope for the future is to find a complete cure for scleroderma. While that goal is still ahead, the continuous dedication of scientists, doctors, and patient advocates means that the journey of understanding and treating this condition moves forward every day. This ongoing work means a lot to those affected by the disease.
Frequently Asked Questions About Scleroderma's Past
When was scleroderma first discovered?
The very first clear description of symptoms that match scleroderma appeared in 1753. This account was given by Dr. Carlo Curzio, who wrote about a young woman with very hard and tight skin. Before this, there were only vague mentions in ancient texts, which are not specific enough to be certain they were about scleroderma. So, you know, 1753 is generally considered the start of its recognized history.
Who first described scleroderma?
Dr. Carlo Curzio is credited with providing the first detailed medical description of a case that is widely recognized as scleroderma. This happened in 1753. Later, Jean-Louis Alibert gave the condition its name, "sclerodermie," in 1817. Both individuals played very important roles in bringing this condition into medical focus. They really helped to shape our early understanding.
What was scleroderma originally called?
Before Jean-Louis Alibert coined the term "sclerodermie" in 1817, there wasn't a single, universally accepted name for the condition. It was often described by its symptoms, such as "skin hardening" or "hide-bound disease." Alibert's name was the first formal medical term that stuck. It was a clear and descriptive name, which is why it became widely adopted, obviously.
Conclusion
The history of scleroderma is a compelling story of persistent observation, scientific inquiry, and growing empathy. From those initial, uncertain glimpses in ancient times to the sophisticated genetic research of today, our understanding of this condition has come an incredibly long way. This journey shows the dedication of countless individuals who sought to unravel a medical mystery.
Knowing this history helps us appreciate the progress made and also highlights the ongoing need for more research and support. It reminds us that medical knowledge is always evolving, and what was once unknown becomes clearer with time and effort. This continuous learning is vital for everyone affected by scleroderma.
If you or someone you care about is living with scleroderma, learning more about the condition can be very empowering. You can learn more about scleroderma on our site, and we encourage you to explore resources for support and current research. Your journey with scleroderma is part of this unfolding history, and understanding its past can help you feel more connected to the present and future of care.
Reference: My text
External Reference: Scleroderma Foundation - History of Scleroderma
Skin Manifestations of Scleroderma, by Dr. Lorinda Chung MD
Scleroderma - Myositis Support and Understanding
The History of Scleroderma | Scleroderma News